Background
Client: Mr. S. – 46-year-old male.
Diagnosis:
- End stage kidney disease (not palliative), on haemodialysis 3x/week
- Peripheral neuropathy
- Right below-knee amputation 2016
- Left below-knee amputation 2017
- Type 2 diabetes mellitus, poorly controlled
- Diabetic retinopathy
- Hypertension
History:
Mr. S. is a 46-year-old man who lives alone in his own home. Despite being unable to work, Mr. S. was mobile, independent and active. In December 2016 a toe on his right foot was amputated due to gangrene. His right leg was subsequently amputated below the knee due to infection and non-healing of the toe wound.
In May 2017 the left leg was amputated below the knee due to a non-healing and necrotic left heel ulcer. Mr. S. was in considerable pain due to the ulcer. With significant small vessel foot disease and no revascularisation options Mr. S. elected to have the amputation.
Other Relevant Information:
Mr. S. was issued with a basic selfpropelling manual wheelchair and basic flat foam cushion following his first below-knee amputation. It was hoped that Mr. S. would be fitted with a prosthesis after healing of the stump and that he could return to independent mobility. This goal was not fulfilled due to very slow healing of the stump wound after amputation of the left leg below the knee.
A clinical case by:
Fiona Smith – Occupational Therapist HBDHB
Megan Ransley – Sales Area Manager – Physiotherapist
New Zealand 2017
Problem
Description of the problem(s):
- The manual wheelchair issued to Mr. S. was not meeting his physical and functional needs. Mr. S. was unable to self-propel effectively due to poor configuration of the wheelchair.
- Mr. S. demonstrated poor sitting posture in his wheelchair. He sat in posterior pelvic tilt and explained that he felt like he was sliding forward in the seat. Upon assessment it was identified that Mr. S.’s posture was fully flexible. The canvas back support and seat had become slung and were further exacerbating this poor posture.
- Mr. S.’s wheelchair cushion was not affording him sufficient pressure redistribution. Mr. S. reported a sitting tolerance of approximately 1 hour before he would experience pain under both ischial tuberosities (ITs) and in his sacral region. Mr. S. can weight shift independently however despite this, Mr. S. reported that he could not comfortably sit in his wheelchair all day and needed to transfer onto alternative surfaces to reduce his discomfort. This limited the activities that Mr. S. could participate in and make it difficult for him to go out all day.
What actions were taken/treatment was tried to solve the problem(s), before the start of this Clinical Case Study?
An attempt was made to reconfigure the manual wheelchair to better meet Mr. S.’s needs. The rear wheels were brought forwards to enable improved access to the push rims, and the front and rear seat to floor heights were altered to enable safer transfers. These changes were insufficient to enable Mr. S. to sit all day and function adequately in his wheelchair.
Solving the problem by use of pressure and shear force measurement
What was the treatment plan/which actions were taken at the start of this Clinical Case Study to solve the problem(s)?
- Mr. S. was issued with a TA-iQ front wheel drive power wheelchair with tilt and HiLow. This wheelchair enabled Mr. S. to access his home and community independently without the fatigue he experienced while self-propelling. The front wheel drive configuration allowed for future proofing of foot placement for prosthetics, which would be explored at a later date.
- A firm and contoured back support was fitted – nxt Active Contour Height adjustable backrest – which assisted
Mr. S. to sit upright without slumping. - Trial of a Vicair Active 9 cushion and a Vicair Adjuster 12 was undertaken.




Pressure Mapping
Undertaken on all three cushions. The single peak pressures seen over the ITs sitting on the foam cushion were eliminated as the legs could be used as weight bearing surfaces.
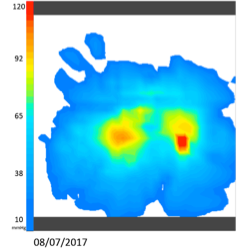
Pressure mapping of the foam cushion demonstrated that Mr. S. was weight bearing significantly through both ITs, but in particular the right with a peak of pressure seen there. It also demonstrated that Mr. S.’s weight was unevenly distributed with almost no weight being taken through the thighs. The picture showed a small surface area of weight bearing. This cushion allowed only one hour of sitting before pain was experienced in the ITs. It is likely that over time the foam was compressing and the cushion’s pressure redistribution properties were diminishing.
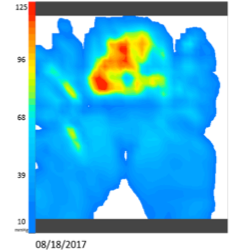
It was thought that the firm front of the Vicair Active 9 would enable safer and easier transfers, while affording the pressure redistribution Mr. S. required. As can be seen from the pressure mapping images, significant improvement was made in relation to the pressure redistribution with a much larger surface area taking weight. This cushion was adjusted by removing 5 cells from both left and right compartment to allow immersion. Mr. S. commented that the cushion felt comfortable and supportive. He sat well with an improved upright posture. He managed to transfer with ease.
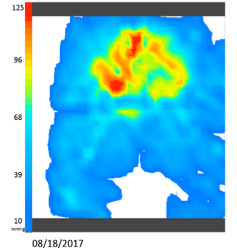
Trial of the Vicair Adjuster 12 cushion was carried out as a comparison. Mr. S. immediately commented that this cushion felt even more comfortable. This is likely because of the depth of the cushion. Mr. S. is a heavy man and could immerse deeply into the Adjuster 12 cushion without the need for cells to be removed. This deep immersion afforded a greater surface area over which his weight was distributed, giving even pressure redistribution and the feeling of greater comfort. The greater immersion available from the Vicair Adjuster 12 cushion also enabled Mr. S. to feel more stable within his wheelchair. The pre-ischial bar provided a barrier to the pelvis sliding forward.
Shearing force
Measured using iShear. This demonstrated that Mr. S. was experiencing not only downward pressure, but also dangerous forward shearing forces (sliding force). Shear forces were reduced from 125.5N on the foam cushion, to 83.2N on the Active 9 cushion, then to 62.2N on the Adjuster 12 cushion. This demonstrates that Mr. S. was able to sit more upright, with less sliding forward. The reduction in shear force is likely contributing to the preference towards the Adjuster 12 cushion the increased comfort and to improved sitting tolerance.
Conclusion
The Vicair Adjuster 12 cushion afforded the high pressure redistribution properties Mr. S. required to sit safely and
comfortably all day. The pre-ischial bar prevented forward sliding of the pelvis, while the deep immersion into the cushion provided stability. The cushion is maintenance free and easy to understand. The Vicair Adjuster 12 cushion was the ideal product choice for Mr. S.’s needs.
Results
What are the results of this new treatment/actions?
Since using the powered wheelchair with Vicair Adjuster 12 and nxt backrest:
- Mr. S. is able to remain comfortably sitting in his wheelchair for the duration of the day.
- Mr. S. can use his wheelchair without the risk of pressure and shear related injury.
- Mr. S. is able to safely and independently access his home and community.